Understanding Osteoporosis and Its Treatment
Discover everything you need to know about osteoporosis and its treatment—from causes, symptoms, and risk factors to proven lifestyle changes.
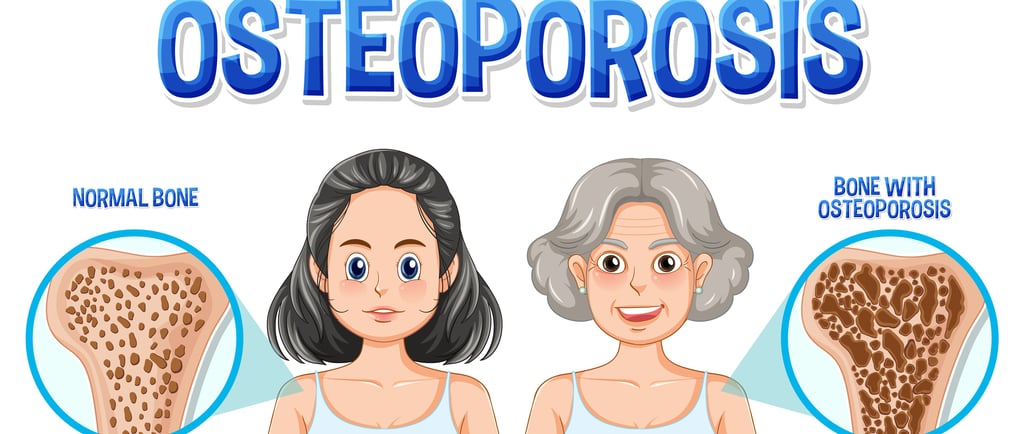

Osteoporosis is a progressive condition that causes bones to gradually weaken and become more fragile over time. The word "osteoporosis" literally means "porous bones," which perfectly describes what happens to your skeletal system as you grow older. Your bones become less dense, develop larger gaps and spaces within their structure, and lose their strength and hardness with time. This deterioration makes even minor falls or bumps serious threats, as your bones can fracture with the slightest trauma.
At any given moment, your body is naturally breaking down old bone tissue and building new bone tissue through a continuous process called bone remodeling. When you're young, new bone is created faster than old bone is removed, so your overall bone mass increases. Most people reach their peak bone mass around their late 20s. After that point, bone remodeling continues, but you lose slightly more bone mass than you gain.
Osteoporosis develops when bone loss occurs too quickly or when bone formation happens too slowly. This condition is often called a "silent disease" because bone loss happens without any noticeable symptoms. Many people don't realize they have osteoporosis until they break a bone from a minor fall or accident. Unfortunately, by that time, significant bone damage had already occurred.
Who Is Most Likely to Develop Osteoporosis?
Osteoporosis affects millions of people worldwide, though certain groups face significantly higher risk. Of the approximately 10 million Americans with osteoporosis, at least 80 percent are women. Women face greater vulnerability primarily due to two factors: they naturally have lighter, less dense bones than men, and they experience dramatic hormonal changes after menopause.
Estrogen, a hormone that helps maintain bone density, drops significantly during and after menopause. During the first 5 to 10 years following menopause, women can lose about 2.5 percent of their bone density every year. That amounts to losing as much as 25 percent of total bone density during this vulnerable period. After menopause, bone breakdown accelerates dramatically, and the creation of new bone slows substantially, triggering the cascade that leads to osteoporosis.
However, osteoporosis isn't exclusively a woman's problem. Men can develop the condition too, though it typically occurs at an older age. Osteoporosis can impact anyone, regardless of their race or age, but some groups, especially those of white and Asian descent, seem to have higher rates of it.
Risk Factors for Osteoporosis
Knowing the risk factors for osteoporosis can help you figure out how likely you are to develop it and what steps you can take to prevent it. Some of these factors are beyond your control, but others are totally manageable.
Non-modifiable risk factors are basically things you can't change, like your genes, age, gender, and family history. If your mom or grandmother dealt with osteoporosis or had a hip fracture, that can really bump up your risk factor. In fact, genetics can explain up to 80% of the differences in how strong our bones are! As you get older, the risk tends to go up, too. Plus, if you’ve had a bone fracture from something that seemed pretty minor, it’s a good indicator that your bones might not be as strong as they should be.
Modifiable risk factors represent areas where you have real power to make changes. One major factor is how much calcium you’re getting. Eating a diet low in calcium dramatically increases your osteoporosis risk because your body can't maintain bone density without adequate calcium. Then there's vitamin D, which is super important too. It helps your body absorb calcium. So, even if you're eating enough calcium, without enough vitamin D, your body won't be able to make good use of it.
Equally important is physical activity. Bones are living tissue that respond to stress, so weight-bearing exercise—like walking, jogging, dancing, or strength training—signals the body to build more bone tissue. Without regular movement, bones lose density faster because they aren’t being “challenged” to grow stronger.
Lifestyle habits are another crucial risk factor for osteoporosis. Smoking is a big problem because it messes with hormone production and cuts down blood flow to your bones, making it harder for them to heal. Drinking too much alcohol can also get in the way of how well your body absorbs calcium and makes vitamin D. Plus, when you throw in a lack of exercise, your chances of developing osteoporosis go up even more.
Additional risk factors to watch out for are being on certain long-term medications like corticosteroids, having a low body weight or being underweight, dealing with chronic health issues like rheumatoid arthritis, inflammatory bowel disease, kidney problems, or hyperthyroidism, going through intense stress, and not eating well overall.
How Doctors Diagnose Osteoporosis
Osteoporosis is often called a silent disease because you may have no symptoms, even as your bones weaken. This makes screening and early detection critically important, ideally before any fractures occur.
The standard test for diagnosing osteoporosis is a bone mineral density test called dual-energy x-ray absorptiometry, or DXA (also called DEXA). This painless, quick procedure takes just 10 to 30 minutes and involves lying on a table while a scanner measures bone mineral density in your lower spine, hips, and sometimes other areas. DXA produces very little radiation—less than one-tenth of a standard chest x-ray and less than a single day's natural environmental radiation exposure.
The test generates a number called a T-score, which compares your bone density to that of a healthy young adult of your same gender. Understanding your T-score is straightforward:
T score > −1: Normal bone density.
T score between −1 and −2.5: Low bone mass (osteopenia).
T score ≤ −2.5: Osteoporosis.
Osteoporosis Treatments
Once you find out you have osteoporosis, there are a bunch of treatment options to consider. Your doctor will help figure out the best plan for you based on how likely you are to have a fracture, your overall health, whether you can take certain medications, and what you prefer.
Medication Treatments
Bisphosphonates represent the first-line and most cost-effective medication option for osteoporosis. These drugs work by slowing bone loss and have been extensively studied and proven effective. Common bisphosphonates include alendronate (Fosamax), risedronate (Actonel), ibandronate (Boniva), and zoledronic acid (Reclast). For most postmenopausal women and men with osteoporosis who haven't experienced prior fractures, alendronate, risedronate, zoledronic acid, or denosumab are appropriate first-line choices.
Oral bisphosphonates like alendronate and risedronate are inexpensive, safe for long-term use, and effective at preventing fractures. However, they can cause side effects, including nausea, heartburn, and esophageal irritation, particularly if not taken with proper precautions.
Denosumab (Prolia) has emerged as an effective alternative to bisphosphonates, particularly for women at high fracture risk or those who cannot tolerate bisphosphonates. This medication works through a different mechanism than bisphosphonates and may provide superior fracture prevention compared to bisphosphonates. Denosumab doesn't get metabolized by the kidneys, making it an excellent option for people with chronic kidney disease. It's administered as an injection just under the skin every six months, eliminating the need to remember daily medications. Like bisphosphonates, denosumab very rarely can cause jawbone damage (osteonecrosis of the jaw) and atypical femur fractures with long-term use.
Hormone Replacement Therapy (HRT) can strengthen bones and is as effective as other osteoporosis medications at preventing fractures in postmenopausal women. Estrogen-containing HRT works by replacing the estrogen that decreased during menopause, helping to slow bone loss. However, HRT carries its own set of potential side effects and health considerations, so it's not appropriate for everyone. Your doctor can help determine whether HRT is a good option for you.
Anabolic medications such as teriparatide (Forteo) and abaloparatide (Tymlos) work differently from other osteoporosis drugs—they actually build new bone rather than just slowing bone loss. These medications are particularly valuable for patients at high fracture risk or those who cannot tolerate other treatments. However, they are generally more expensive and come with more side effects, including dizziness, headaches, and leg cramps.
Lifestyle Modifications
While medications can be highly effective in treating osteoporosis, your lifestyle choices are equally—if not more—important in maintaining long-term bone strength. Healthy bones thrive on regular movement, good nutrition, and mindful daily habits that protect against falls and injuries.
Let’s start with exercise, which is one of the most powerful, natural ways to strengthen bones. Bones adapt to the stress placed upon them, so when you engage in weight-bearing exercises—like walking, hiking, dancing, or light jogging—you’re essentially signaling your body to make bones stronger and denser. Add to that strength-training exercises, such as lifting light weights or using resistance bands, and you’re working the muscles that support your bones, improving balance and coordination in the process.
Next comes diet, which serves as the foundation for strong bones. Your bones act as mineral storage for your body, and when your diet lacks key nutrients—particularly calcium and vitamin D—the body will draw these from your bones, weakening them over time. To prevent that, include calcium-rich foods like milk, yogurt, cheese, tofu, almonds, and leafy greens in your meals. Vitamin D, which helps the body absorb calcium efficiently, can be obtained through safe sun exposure, fatty fish like salmon, fortified cereals, and supplements if necessary.
Beyond diet and exercise, avoiding harmful habits is just as critical. Smoking can reduce blood flow to bones and lower estrogen levels in women, accelerating bone loss. Excessive alcohol intake interferes with calcium absorption and affects the body’s ability to produce vitamin D, further compromising bone health. Moderation or complete avoidance of these substances significantly lowers your risk of osteoporosis-related fractures.
FAQs About Osteoporosis and Its Treatment
1. Can osteoporosis be reversed?
While bone loss can’t be fully reversed, treatments can stop its progression and strengthen existing bone.
2. Who should get a bone density test?
Adults over 50 and postmenopausal women are most commonly advised to have one.
3. Is osteoporosis only a women’s disease?
No, men can develop it too, especially with aging or long-term medication use.
4. What’s the best natural way to improve bone density?
Weight-bearing exercise and a calcium- and vitamin D-rich diet are very crucial to be integrated in everyday life.
5. Are supplements effective?
They can help fill nutritional gaps but shouldn’t replace a healthy diet.
Conclusion
Osteoporosis might sound scary, but it doesn’t have to control your life. By understanding what is osteoporosis and its treatment, you’re already taking a big step forward. With the right combination of early diagnosis, appropriate medical care, and smart lifestyle choices, you can protect your bones and maintain your strength